01 Jun Let’s Talk about Your Sleep Apnea
Hi I’m Dr. Erika Mason. I want to go over today some things I review with patients about their sleep study, what sleep apnea is, what we are counting and how it affects you.
I wanted to start first with Mr. AirHead. Mr. AirHead will demonstrate what happens when we have sleep apnea. When we are awake we never stop breathing. Our brain is “Johnny on the spot” and it tells us “Breathe, breathe, breathe.” We don’t give it another thought. But when we lay down, either on our back or on our side, what happens is the brain is sleeping too and that’s the problem. When our jaw drops back and blocks the airway, we can try to breathe through our nose or try to breathe through our mouth but nothing is happening. There is a delay before the brain actually picks up on that you are not breathing.

The first thing our body does is the brain says, “Oh, let’s send a signal and move your leg.” You aren’t waking up but the brain woke up. The brain sends signals that are sent to the legs and the legs will move, and that will arouse you enough to move. The And so, you will take a breath and you will be fine and then your jaw will drop back again. The brain then notices you are not breathing again and sends more signals and the next signal might be to roll over. The brain then notices that you aren’t breathing again and then sends more signals to move you. This is how we end up tossing and turning from side to side throughout the night. And most people say, “oh, well it was my hip, it was my shoulder. I have some aches and pains.”
Well, that might be true, but it’s mainly the brain trying to keep you alive and luckily it is nudging you throughout the night to be able to take a breath. So, one way of treating this is that we can put on a mask and blow continuous positive air pressure. So, when the mask is on and it starts blowing, we turn up the pressure enough that it pushes around the obstruction, giving you air into your lungs. So, that is CPAP, continuous positive air pressure. Or with an oral appliance, we just put this little piece of plastic in between your teeth and it holds your jaw from collapsing. So, it’s really pretty easy. So, put that appliance in, that airway is open of your windpipe, and then we pick an appliance that we can move forward. So, it’s a very simple fix. If we need to have your jaw to move a little bit more, we pick an adjustable appliance that can advance your lower jaw a little bit more forward if we need to enhance the airway.

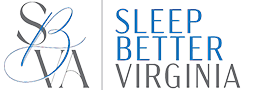
We start by looking at your sleep study that diagnosed your sleep apnea. Obstructive sleep apnea is one of 90 sleep disorders. It’s the only one that I treat and am certified to treat. Sleep physicians will diagnose and treat the other 89. When we have sleep apnea, we are counting during the study some different things. And so, I’m still going to use Mr. Airhead here to explain what they are, but we’re counting what’s called an apnea and a hypopnea. An apnea is a total collapse of one’s airway and it starts counting after you have stopped breathing for 10 seconds or more and it’s usually more.
So, we have that as part of the sleep study. The other thing that counts is what is called a hypopnea. And a hypopnea is a flow problem. So, if your jaw and your tongue fall back and block the flow of air by 50 percent or more in a window of time of 10 seconds or more, then it’s scored as a hypopnea. I use the analogy of a garden hose. If you turn the garden hose on and no water is coming out, or there’s an actual knot in the garden hose, that’s an apnea. You aren’t getting any water out. If you fix the garden hose and now the flow of water is fine but you pull the garden hose to water another flower, and it hooks on a chair on your deck. As it hooks on that chair on your deck, it squishes the actual hose and only lets out a little bit of dribbling of water and that’s what I would consider a hypopnea.
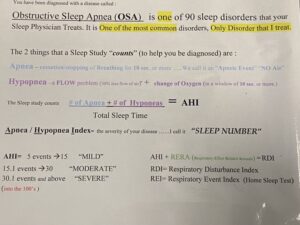
Those are two problems: apnea is no air and hypopnea is a decreased amount of air. You’re still getting air, but it’s 50% less. So, that’s my analogy. What we’re doing is counting those, totaling them all up for the whole night or the eight hours that you slept or six hours, and then dividing it by either your monitoring time, meaning you turn on the home sleep test and then turn it off, or we know whether or not you have gone to sleep and when you wake up. So, the total sleep time. We do the math and that gives us what we call the apnea/ hypopnea index. The apnea/hypopnea index, I call it your sleep number. If you have five events in an hour, you’re diagnosed with obstructive sleep apnea.
Mild, moderate, and severe sleep apnea are defined by the sleep study number: 5 to 15 is considered mild, 15.1 to 30 is considered moderate, and then anything over 30.1, even into the hundreds is considered severe. But those aren’t really part of what we need to know because that’s more of an insurance thing. Most people say oh, well I have mild sleep apnea, so do I really need to treat it? Well, I use the analogy again of well, when you get diagnosed, it’s similar to oh, are you pregnant or not pregnant? It has to be treated. So, it doesn’t matter whether it’s mild, moderate, or severe, it needs to be treated. This is a quick overview of what a sleep number or your index is and what those numbers mean. Moving on when we look at a sleep study and I’m going to show you here, the sleep study will tell us your body position. It will tell us heart rate. It will tell us oxygenation.
If you’re holding your breath, for example, with the apnea and hypopnea, then your oxygenation is going to start wavering and we use the term desaturating. Our cutoff usually is at 88 when people’s oxygenation when they’re sleeping or conserving energy. It usually is in the low nineties, if you’re running around and during the day you take your oxygenation, it’s probably 98, 99, or a hundred percent. But when you’re sleeping, it should be in the low nineties, like 92, 91, 94. But we don’t want it to go below 88%. Now some sleep physicians score it at 89, some score it at 90, but the majority of people or sleep physicians have the cutoff at 88. And so, under 88 that’s a bit concerning. Like if you were in a outpatient sleep facility and had come out of surgery and you have a pulse oximeter on your finger, if it dropped below 88 then the alarm would be going off to tell the nurse to come and check on you.
It’s pretty important for our oxygenation to be 88 and above. So, then usually it tells us what type of events that you’re having. These are apnea and these are hypopnea. And you can see as the night progressed, they got better. This particular study was showing us, moving their jaw more forward and resolving their issues by moving their jaw more forward. Then this line is telling us the different staging of sleep. This is an in-lab study that’s called a PSG. Sometimes when we do a home test, the sleep test will kind of guesstimate what different stages you’re going into and they base it on how active you are in the bed, which is called actigraphy. But it’s kind of still a bit of a guess, it’s not like you have the electrodes on your brain knowing whether you are asleep or awake and that’s called an EEG. So, this is kind of just what I will go over or your sleep position has gone over for the diagnosis of sleep apnea.

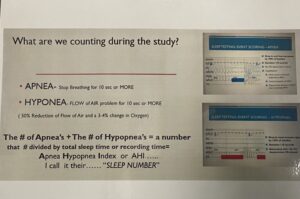
The next thing that I would like to talk about is some of your anatomy. So, when I do the cone beam scan, I will be plotting out how narrow your airway is. There’s different levels of the airway. So, the top part is considered well, this one is called the nasopharynx. Then a little further down is the velopharynx. And then part of the oral mouth part is called the oropharynx. And then the last part is called the hypopharynx. So, there’s different levels of the wind pipe or the airway. So, when I map out, it’s usually this oropharynx that I’m mapping out and most patients without sleep apnea have an airway of 20 or above. But most of my patients, when I do the cone beam scan and map it out, it’s 10 or below. So, it’s like half. And so, the culprit is usually the jaw falls back and blocks the airway, just like I showed with Mr. Airhead.
The next thing that I wanted to talk about is how I pick an appliance. So, this is a micrograph looking under a microscope at different appliances and what the material looks like at a hundred microns under the microscope. And to me, that’s pretty important because some are handmade, so there’s a lot of big holes and porosity is what we call it, so that bacteria, biofilm, gunk can get in there and then that deteriorates the appliance over time. This particular appliance actually is very consistent, it’s prefabricated. And so, liquid and powder are put into these forms and actually it looks like this puck. And so, technology’s being used so that the puck of plastic is more consistent. Therefore, it’s stronger. Therefore, they can make the footprint smaller. And in this particular case, the manufacturer actually uses technology to cut it out like cutting out a key like at Lowe’s or something. So, or trying to eliminate the human error.
And when you have appliances that are handmade, there is more of a capability of having them stain and have possibly mold or bacteria or bio gunk in there and breaking them down. The other thing that I’m showing here are printed nylon. These are 3D printed appliances that are made out of a poly nylon, but tend to have a lot of porosity as well. So, you can see that the big holes happen. And so, there were a few of those on the market. One company has left and gone back and only is distributing them in Europe, but they were manufactured in a white color, but over time, fairly quickly they would turn very yellow looking because of that porosity. So, and then this one is kind of in between. It’s not quite as good as the puck of plastic, but it’s a little bit better than one that is actually handmade by a lab technician that sits at a lab bench using liquid and powder to make the appliance. And I think this is important in picking the appliance that would be best for you and different companies and manufacturers use different products.

That is a wrap up of what I would go over with you for a consultation. I’ve talked about Mr. Airhead, how the apnea happens with you blocking it, what a hypopnea is. I’ve talked to you about how the brain wakes up and tries to nudge you to take a breath. I’ve talked about the different sleep numbers and how that happens. I’ve talked about your sleep study and how we come about those numbers, five to of 15 being mild, 15 to 30 being moderate, and anything over severe. But you have to treat any of them because obstructive sleep apnea tends to have some very severe health problems if it’s not treated and managed properly. And then we’ve talked about the different materials that appliances are made out of and how they are manufactured. So, happy sleeping.